Heart attack sufferers can now regain heart function with transplanted muscle cells
02/13/2019 / By Ralph Flores
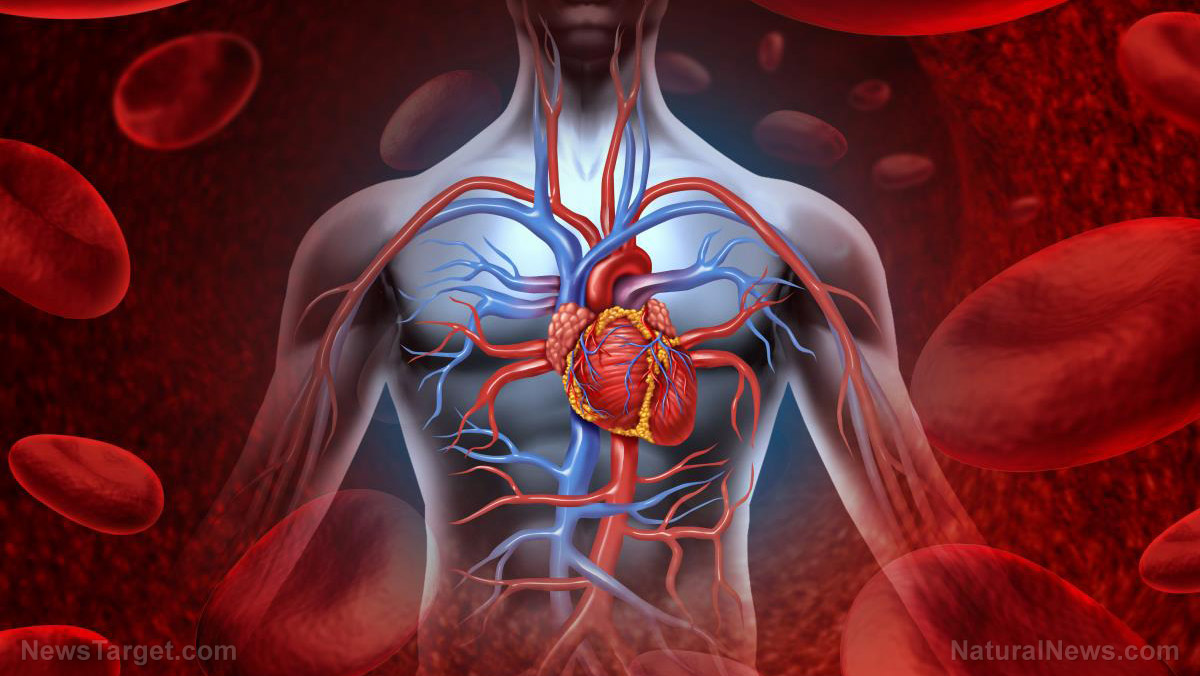
People who have experienced a heart attack are sure to find some form of relief, thanks to the efforts of researchers from the University of Bonn. In the study, titled “Improved heart repair upon myocardial infarction: Combination of magnetic nanoparticles and tailored magnets strongly increases engraftment of myocytes,” researchers exhibited a procedure to repair cardiac tissue after a heart attack using replacement muscle cells containing magnetic nanoparticles. These cells are then injected into the damaged area of the heart and are held in place by a magnet – which helps the nanoparticle-containing cells to engraft better to existing tissue. This procedure, in turn, may lead to a “significant improvement in heart function.”
The cardiac tissue is known to be an extremely specialized muscle. As the name implies, this type of tissue is solely located in the heart and immediately starts beating as soon as it is formed. However, this trait is also a challenge. In the wake of heart attack, some cells in the cardiac tissue are damaged due to the formation of clots – which deprived them of oxygen and other nutrients found in the blood. Repairing these muscles has proven to be tricky, as any replacement muscles are pushed out of their intended channel due to the heart’s continuous pumping action. With only a few cells attached to the cardiac tissue, the amount of repair is just limited.
This challenge was the primary objective of the study, as researchers conducted in vivo studies on mice to determine the efficacy of the procedure. For the study, mice that had previously suffered a heart attack were grafted with replacement muscles that were outfitted with magnetic nanoparticles. The sample pool was divided into an experimental group, which also placed a magnet a few millimeters from the surface of the heart, and a control group, which only had the muscle graft.

The results showed that the group which had magnets in place were able to keep more of the transferred cells over than those without it. The experimental group was able to retain 60 percent of the replacement cells settled in the target area. In comparison, the control group only had 25 percent of its replacement cells intact. Moreover, the effect of the magnetic field was immediate: Researchers observed that the cells that were under the magnetic field remained at the target site 10 minutes after the procedure. The cells continued to do so on the succeeding days until they were able to attach themselves to existing cardiac tissue.
The team was also surprised that the transplanted cells did not immediately die, instead, they were able to graft themselves into the cardiac tissue and multiply. This, researchers suggested, could be due to a more intensive cell-cell interaction between the transplanted cell and the tissue. This translated to better cardiac function in the experiment group that used magnets.
Researchers indicated that while the study has been successful in mice, the procedure has the potential to move into human treatment. Still, the research team has noted that actual clinical testing on human needs further studies. (Related: Magnet Therapy Works as a Healing Tool.)
Earlier studies have explored the capability of nanomagnets in repairing damage to other parts of the body. A study conducted by the University College London showed that nanomagnets could be used to deliver stem cells to injury sites, thereby improving the capacity of cells in repairing tissue that was damaged.
Sources include:
Submit a correction >>
Tagged Under:
cardiac tissue, Heart, heart attack, heart health, magnetic particles, transplant
This article may contain statements that reflect the opinion of the author