Health Freedom vs. The Mandate: $8B Vaccine industry fights to keep injecting every American at birth
12/06/2025 / By Willow Tohi

- The CDC’s vaccine advisory panel is poised to vote on a proposal to end the universal hepatitis B vaccine birth dose for infants of negative-testing mothers.
- A preemptive media and op-ed campaign, led by former health officials, warns this change could reverse decades of progress, predicting a modest increase in infant infections.
- Critics argue the universal policy is a “temporal mismatch,” vaccinating millions of low-risk newborns against a primarily adult-transmitted disease to catch a small number of missed maternal cases.
- Significant safety concerns, particularly regarding the 250-microgram aluminum adjuvant injected into newborns, are highlighted as being omitted from the defense of the current policy.
- The debate underscores a core conflict: a public health strategy of mass vaccination versus a more targeted approach centered on improved and rapid maternal testing.
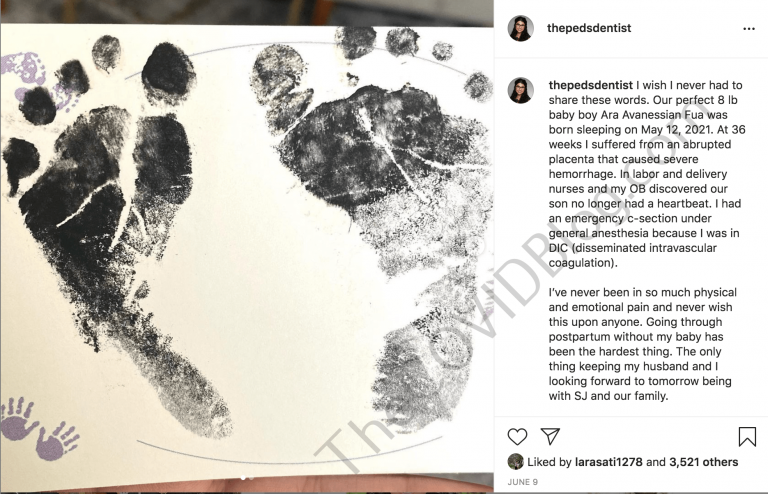
The Centers for Disease Control and Prevention’s (CDC) vaccine advisers are preparing to vote on whether to rescind the 34-year-old mandate that every newborn receive a hepatitis B vaccine within 24 hours of birth. This pending policy change has ignited a fierce public relations battle, pitting former top health officials defending the universal mandate against medical skeptics and health freedom advocates who argue the policy represents an outdated and potentially risky overreach. The clash centers on a fundamental question: Is it ethical to universally vaccinate healthy newborns against a disease they have virtually no risk of contracting, for the sake of catching a tiny fraction of missed cases?
The establishment’s preemptive strike
Ahead of the pivotal Advisory Committee on Immunization Practices meeting, a coordinated media effort has emerged to defend the status quo. An op-ed in the Journal of the American Medical Association, authored by former CDC Director Dr. Rochelle Walensky and other establishment figures, warned that removing the universal birth dose could lead to dozens more infant hepatitis B infections annually. Major news outlets have echoed this stance, framing the proposed change as a dangerous concession to vaccine hesitancy. Their argument rests on modeling that suggests the current policy acts as a “critical safety net,” primarily to prevent transmission from the small number of mothers whose infections are missed by prenatal screening or who contract the virus late in pregnancy.
A question of risk and “temporal mismatch”
Critics of the universal policy challenge its very foundation, calling it a profound “temporal mismatch.” They note that hepatitis B is primarily transmitted through intimate contact or shared needles, with the highest risk periods occurring in adolescence or adulthood. The central justification for the birth dose is preventing perinatal transmission from an infected mother. However, with less than half of one percent of pregnant women in the U.S. testing positive, they argue that subjecting 3.6 million newborns annually to a medical intervention is disproportionate. The more direct solution, they contend, is not universal vaccination but universal and rapid point-of-care testing for mothers at delivery, a method used successfully in other countries to identify the truly at-risk infants without injecting the vast majority who are not.
The aluminum elephant in the nursery
A glaring omission in the op-ed and media defense of the hepatitis B vaccine, according to policy analysts, is any substantive address of aluminum adjuvant safety. The U.S. birth dose contains 250 micrograms of aluminum. Pediatricians like Dr. Paul Thomas have pointed out that this single injection exceeds the FDA’s maximum recommended daily aluminum exposure for a newborn by more than tenfold. While promoters cite studies affirming the vaccine’s safety, skeptics note that these often reference research from countries with lower aluminum exposure schedules and do not account for the cumulative aluminum load from the entire U.S. childhood vaccine schedule. The concern is that injected aluminum, a known neurotoxin, can cross the blood-brain barrier during a critical period of neurological development, with potential long-term consequences that have never been comprehensively studied by the CDC.
Profit, policy and parental choice
Beneath the medical debate lies a stark economic reality. The global hepatitis B vaccine market is valued at over $8 billion. A move from universal vaccination to a targeted strategy based on maternal testing would undoubtedly impact this market. Critics argue this financial incentive helps explain the resistance to policy change, framing the universal mandate as a profitable “one-size-fits-all” solution that bypasses informed consent. They emphasize that vaccines, unlike treatments for the sick, are given to healthy populations, imposing an exceptionally high ethical burden to prove both necessity and safety—a burden they believe has not been met for the universal newborn hepatitis B shot.
A pivotal moment for vaccine policy
This week’s vote represents more than a schedule tweak; it is a referendum on a core philosophy of American public health. The outcome will signal whether the system retains its rigid commitment to mass, age-based vaccination mandates, or begins a shift toward more personalized, risk-based medicine that weighs individual patient circumstances. For parents, it is a rare moment of potential agency in a process often experienced as coercive. The decision will determine if the newborn nursery remains a place where the first medical act is a state-mandated injection for a disease of adulthood, or if the door opens to a more nuanced approach that prioritizes immediate testing and truly informed choice.
Sources for this article include:
Submit a correction >>
Tagged Under:
. vaccines, Aluminum, bias, Big Pharma, CDC, Fact Check, health freedom, infant health, informed consent, media fact watch, pharmaceutical fraud, poison, propaganda, real investigations, toxic ingredients, toxins, vaccine wars
This article may contain statements that reflect the opinion of the author