Is this the next superbug? Understanding drug-resistant candida and why antibiotics don’t work
07/29/2018 / By Ralph Flores
Move over, superbug: The next drug-resistant pathogen could be a fungus that already calls our body home.
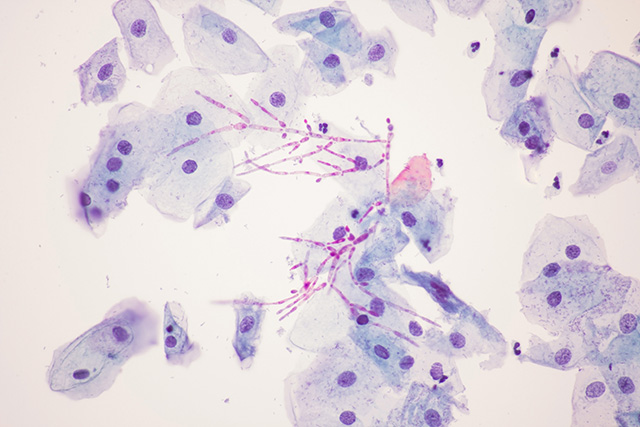
In a study published in The Journal of Infectious Diseases last year, researchers noted an uptick in reports of invasive Candida infections that are resistant to antifungal agents. The article, which discussed the current trends in multidrug resistance, revealed that cases of multidrug-resistant C. glabrata are now common in many health centers. Surprisingly, reports of resistance increased with the introduction of more antifungal agents, including azoles which were known to be especially effective against Candida species.
To understand the underlying mechanism behind this dangerous multi-drug resistance, Charles Kwang of Kwang Wellness walks us through how Candida affects a person’s body, why conventional treatments are useless against it, and what we can do to prepare against it.
Watch the full episode from Brighteon.com here:
Uncovering a dangerous pathogen
“There is no test to prove Candida,” Kwang explains in his video. “No medical doctor’s ever going to diagnose Candida.”
In most cases, the patients will discover that they are infected with Candida on their own. For the most part, a person that suffers from a condition – this includes anything from food allergies to chronic obstructive pulmonary disease (COPD) – with an undetermined cause could be candidates for a Candida infection.
“Any health problem that has no cause – most likely, there is a cause,” he added.
The power of the elements: Discover Colloidal Silver Mouthwash with quality, natural ingredients like Sangre de Drago sap, black walnut hulls, menthol crystals and more. Zero artificial sweeteners, colors or alcohol. Learn more at the Health Ranger Store and help support this news site.
To understand how Candida affects the body and why is it so virulent, it’s best to look at how conventional medicine uses drugs to treat a certain condition.
Healthcare professionals use antibiotics as a first-line drug to treat a disease. If this doesn’t work, they then prescribe second-line drugs such as steroids.
When both treatments fail, Kwang reveals that so-called “chemo drugs” are used. In rheumatoid arthritis, for instance, healthcare professionals will first start with antibiotics to treat the condition, then move up to steroids, until reaching a point that they will use chemo drugs such as methotrexate, which carries potentially life-threatening side effects.
If a patient who responded well to antibiotics experiences worse symptoms after treatment – “that’s when you know exactly you’re dealing with Candida,” explained Kwang.
So, what makes Candida drug-resistant? That answer, according to Kwang, can be found in why antibiotics were initially created, and how it has developed until now. Antibiotics, to begin with, were designed to get rid of bacteria – that’s why penicillin and amoxicillin were created using the toxins from molds. During the war, antibiotics worked wonders, as they could be used in large amounts to minimize infection. However, doctors have put out stronger medications that were targeted to treat a wider range of pathogens.
“But what if you’re not fighting a bacteria anymore?” Kwang asks. “What if you’re fighting Candida?”
For one, Candida is a relative of yeast and molds – which antibiotics were derived from. This makes it naturally resistant to antibiotic treatments.
This is where the problem becomes progressively worse. While bacteria such as MRSA have shown some level of drug-resistance, these are can still be treated with end-line medication, unlike Candida. The chronic use of antibiotics is also a risk factor for Candida infections, as these indiscriminately kill all bacteria in the body – including good bacteria.
These create the perfect scenario for Candida to survive. Once this happens, it seeps into the system and pulls down the body’s immunity. This renders antibiotics ineffective – which paves the way for more severe bacterial infections. This condition, over time, adds more stress to the immune system as Candida infections do not only strengthen secondary other pathogens, it also creates toxins that overload the body’s defenses (Related: Candida Overgrowth may be affecting your health.)
“You may see that with someone who has an immune system problem,” Kwang said. “There’s Candida underneath that.”
The feature is part of a running series on Candida infections, which can be viewed at this link.
Learn more natural ways to cure Candida by following NaturalCures.news today.
Sources include:
Tagged Under: Antibiotics, candida, candida infections, drug resistance, drug-resistant bacteria, drug-resistant candida, infections, priority, superbug, superbugs